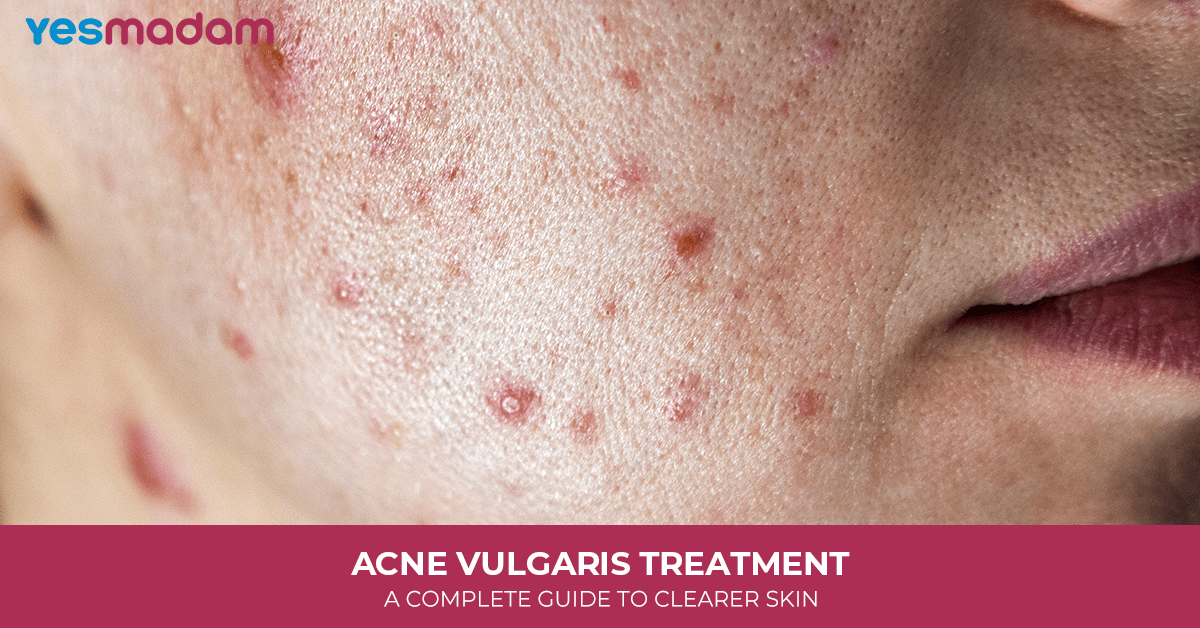
Acne Vulgaris Treatment: A Complete Guide to Clearer Skin
Acne is something most of us have faced at some point, but for many, it’s more than just a passing skin issue. Acne vulgaris treatment is one of the most discussed topics in dermatology because it affects people across ages and lifestyles. From the occasional breakout to severe, persistent acne, the journey to clearer skin often feels overwhelming.
The good news? There isn’t just one solution. Over the years, medical science, skincare research, and even lifestyle shifts have introduced a variety of approaches to managing acne. Whether you’re exploring topical creams, oral medications, advanced therapies, or home-based remedies, there’s a treatment pathway that can fit your needs.
This guide breaks down everything you need to know about acne vulgaris treatment, covering conventional therapies, holistic approaches, and lifestyle tips, so you can make an informed decision about your skin health.
Table of Contents
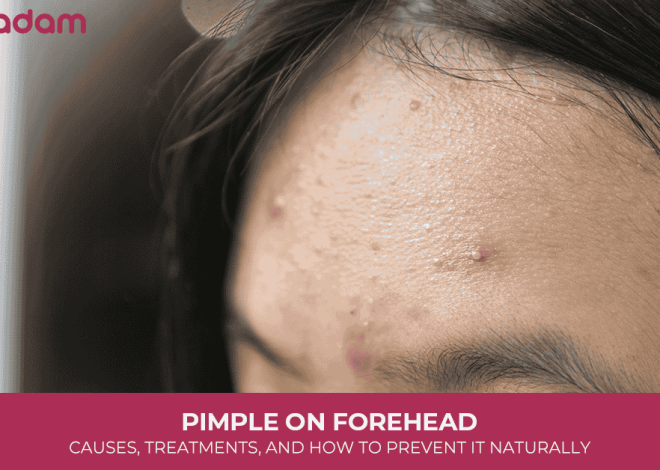
What is Acne Vulgaris?

Before we explore treatments, it’s important to understand what acne vulgaris really is. At its core, acne develops when pores get clogged with oil, dead skin cells, and sometimes bacteria. This leads to blackheads, whiteheads, papules, pustules, nodules, or cysts.
While hormones play a major role (especially during teenage years), factors like genetics, stress, skincare products, and even diet can contribute. The severity of acne varies, and so does the treatment. That’s why dermatologists often personalize acne vulgaris treatment based on the type and intensity of the condition.
What Causes Acne Vulgaris
Acne vulgaris is a common skin condition that develops when hair follicles become clogged. The causes are multifactorial, and usually involve a combination of internal and external factors. Here are the main contributors:
1. Excess Sebum (Oil) Production
- The sebaceous (oil) glands produce too much sebum.
- This excess oil mixes with dead skin cells and blocks pores, creating the perfect environment for acne.
2. Abnormal Shedding of Skin Cells
- Normally, dead skin cells rise to the surface and are shed.
- In acne, these cells may stick together and clog hair follicles, trapping oil and bacteria inside.
3. Bacterial Growth
- A bacteria called Cutibacterium acnes (formerly Propionibacterium acnes) thrives in clogged pores.
- It breaks down sebum, producing substances that trigger inflammation and pus formation.
4. Inflammation
- The body’s immune system reacts to bacteria and clogged pores, causing redness, swelling, and tenderness — the hallmark signs of pimples.
5. Hormonal Changes
- Androgens (male hormones present in both men and women) increase sebum production.
- This is why acne often appears during puberty, before menstruation, in pregnancy, or with hormonal conditions like PCOS.
6. Genetic Factors
- A family history of acne increases the likelihood of developing it.
- Genetics can influence sebum production, immune response, and skin cell behavior.
7. Other Contributing Factors
- Diet: High-glycemic foods, dairy, and excessive sugar may worsen acne in some people.
- Stress: Triggers hormone fluctuations that can aggravate acne.
- Medications: Steroids, lithium, and some anticonvulsants can cause breakouts.
- Cosmetic products: Heavy, oily skincare or makeup may block pores.
- Environmental factors: Humidity, sweating, and pollution can also contribute.
Common Treatments for Acne Vulgaris

Acne vulgaris can be managed with a variety of treatment options depending on its severity, type, and individual skin response. Below are the most commonly used therapies, ranging from topical agents to systemic medications. Each has specific benefits, side effects, and usage guidelines.
Retinoids (Vitamin A Creams & Gels)
Retinoids like tretinoin, adapalene, and tazarotene help unclog pores by speeding up cell turnover. They are considered a first-line treatment for mild to moderate acne. In addition to reducing pimples, they improve skin texture and fade post-acne marks.
Beginners may face dryness, peeling, or redness, so it’s best to start slowly, moisturize well, and use sunscreen. Consistent use usually shows results in 8–12 weeks.
Benzoyl Peroxide (BPO)
Benzoyl peroxide is a powerful antibacterial ingredient that fights Cutibacterium acnes. Unlike antibiotics, bacteria do not become resistant to it, making it a reliable long-term option. It comes in cleansers, gels, and spot treatments.
Side effects mainly include dryness and irritation, which can often be minimized by starting with lower concentrations (2.5%–5%).
Oral Antibiotics
For more widespread or inflamed acne, doctors may prescribe oral antibiotics like doxycycline or minocycline. These reduce both bacteria and inflammation.
They are usually combined with topical treatments to prevent resistance. Antibiotics are generally prescribed for 3–6 months before switching to other long-term options.
Isotretinoin (Accutane)
When acne is severe, scarring, or unresponsive to other treatments, isotretinoin is the most effective option. It shrinks oil glands, clears pores, and lowers bacteria, often leading to long-term remission.
However, it requires strict medical supervision, regular blood tests, and pregnancy prevention measures due to serious potential side effects. Common side effects include dryness, nosebleeds, and, rarely, more severe health risks.
Azelaic Acid
A gentler treatment, azelaic acid has antibacterial, anti-inflammatory, and skin-brightening properties. It’s particularly useful for people dealing with both acne and dark spots from pigmentation.
It is well tolerated by sensitive skin and often paired with stronger acne medications to balance effectiveness with tolerability.
Salicylic Acid
Salicylic acid, a beta-hydroxy acid (BHA), works by unclogging pores, dissolving excess oil, and exfoliating dead skin. It’s especially effective for blackheads and whiteheads.
It’s available in many cleansers and toners. Since it can cause dryness, most dermatologists recommend starting with once-daily use and adjusting based on skin tolerance.
Acne Vulgaris Treatment: DIY Home Remedies
So, you’re dealing with acne and want to try some natural fixes? Good news: a lot of kitchen and garden ingredients can actually help! Let’s break it down step by step.
Step 1: Gentle Cleansing (Keep It Simple)
- Wash your face twice a day with lukewarm water.
- Skip harsh scrubs—they only irritate your skin.
- Try this at home:
- Oatmeal + honey paste → gentle and soothing.
- Or just aloe vera gel → cleans + calms at the same time.
Rule of thumb: be kind to your skin, not aggressive.
Step 2: Spot Treatments (For Pesky Pimples)
- Tea tree oil → dab a tiny bit, but always dilute with a carrier oil.
- Honey + cinnamon paste → works like a natural antibacterial cream.
- Apple cider vinegar toner → mix with water (1:3 ratio). Wipe lightly with a cotton pad.
Patch test first. Some natural stuff can sting or burn if too strong.
Step 3: Calm the Redness
- Aloe vera gel straight from the plant = magic for redness.
- Green tea bag compress → cool, refreshing, and anti-inflammatory.
- Turmeric + honey paste → golden glow + bacteria fighter.
Step 4: Exfoliate (But Not Every Day)
Do this only once or twice a week:
- Sugar + honey scrub (gentle, don’t rub too hard).
- Ground oatmeal + yogurt = creamy exfoliator.
- Coffee grounds + aloe vera = energizing scrub.
Step 5: Eat & Live Acne-Friendly
- Cut down on sugary, fried, and super-processed foods.
- Eat more veggies, fruits, and omega-3 foods (fish, flaxseeds, walnuts).
- Stay hydrated 💧—water helps flush toxins.
- Sleep well and keep stress in check (yoga, meditation, or even dancing around your room helps!).
Step 6: Easy Face Masks
- Fuller’s Earth (Multani Mitti) + rose water → soaks up excess oil.
- Honey + lemon (occasional, not daily) → clears bacteria + lightens scars.
- Cucumber + yogurt → cooling and refreshing.
Step 7: Daily Habits That Matter
- Change pillowcases often (they collect oil and bacteria).
- Don’t touch or pop pimples—seriously, it only spreads them.
- Use a light, oil-free moisturizer—yes, oily skin needs moisture too!
Treat your skin gently, use natural antibacterials like tea tree and honey, calm it with aloe and green tea, exfoliate occasionally, and live a balanced lifestyle. Consistency is your best friend here.
Acne Vulgaris Diet and Lifestyle Changes
Research suggests that what you eat and how you live may influence your skin. While there’s no one-size-fits-all rule, acne vulgaris diet and lifestyle changes can make a real difference.
Some helpful tips include:
- Reducing high-glycemic foods (like sugary snacks or white bread) that spike insulin and trigger breakouts.
- Limiting dairy, especially skim milk, which some studies link to acne.
- Staying hydrated and eating a balanced diet rich in whole foods, omega-3s, and antioxidants.
- Managing stress through exercise, meditation, or proper sleep.
These changes don’t provide overnight results but can improve skin health and overall well-being in the long run.
Laser and Light Therapy for Acne Vulgaris
For those seeking advanced treatments, laser and light therapy for acne vulgaris offers promising results. These therapies target acne-causing bacteria, reduce oil production, and even help with scarring.
Popular options include:
- Blue light therapy: Targets bacteria in the skin.
- Photodynamic therapy (PDT): Combines light with a topical solution for stronger effects.
- Laser resurfacing: Improves both acne and scarring.
While these treatments can be costly, they’re often considered when topical or oral options aren’t enough, or when scarring needs to be addressed.
Conclusion
When it comes to acne vulgaris treatment, there isn’t a one-size-fits-all solution. From topical retinoids and benzoyl peroxide to oral antibiotics, isotretinoin, azelaic acid, and even home remedies, the options are vast. Add to that the role of diet, lifestyle, and modern therapies like laser treatments, and it becomes clear that managing acne is about finding the right combination that works for you.
The journey may require patience and consistency, but with the right approach, clearer and healthier skin is absolutely possible.
FAQs
1. What is the best first-line acne vulgaris treatment?
For most people, topical retinoids or benzoyl peroxide are considered first-line treatments. They target clogged pores and bacteria, which are the root causes of acne.
2. How long does it take for acne treatments to show results?
Most acne treatments take 8–12 weeks before significant improvement is visible. Patience is key, as stopping too early can cause breakouts to return.
3. Can diet really affect acne vulgaris?
Yes, research suggests that high-glycemic foods and dairy may contribute to acne in some people. A balanced diet with whole foods often supports clearer skin.
4. Are home remedies effective for acne?
Home remedies like aloe vera, honey, and tea tree oil can help mild acne but usually aren’t enough for moderate or severe cases. They work best as complementary care.
5. What are the side effects of topical retinoids?
Common side effects include dryness, peeling, and redness. These usually improve as your skin adjusts. Moisturizer and sunscreen help reduce discomfort.
6. Is benzoyl peroxide safe for long-term use?
Yes, benzoyl peroxide can be used long-term. Since bacteria don’t develop resistance to it, it remains effective even after months of use.
7. When should I consider oral antibiotics for acne?
Oral antibiotics are usually considered for moderate to severe inflammatory acne when topical treatments alone aren’t enough. They’re not recommended for long-term use.
8. What makes isotretinoin different from other treatments?
Isotretinoin targets all major causes of acne—oil production, clogged pores, bacteria, and inflammation. It’s the most powerful option but requires strict monitoring due to side effects.
9. Can stress cause acne vulgaris flare-ups?
Yes, stress increases hormones like cortisol, which can trigger oil production and worsen acne. Managing stress can improve both skin and overall health.
10. Is laser therapy a permanent solution for acne?
Laser and light therapies can reduce acne and improve scars, but they aren’t permanent cures. Maintenance sessions may be needed, and combining them with medical treatments often gives the best results.